The Australian College of Optometry (ACO) is proud to announce it has extended bulk billing to all eye examinations for children under the age of 18, with immediate effect from October 30. The public health eyecare provider hopes that the extension will remove any financial barrier to paediatric eyecare.
The change to billing includes all paediatric services including its Children’s Clinic and advanced Myopia and Binocular Vision clinics in Carlton, as well as services provided at the ACO’s seven satellite clinics throughout Melbourne. Established in response to the increasing rate of myopia, the ACO’s Myopia Clinic is the only public health clinic of its kind in Victoria.

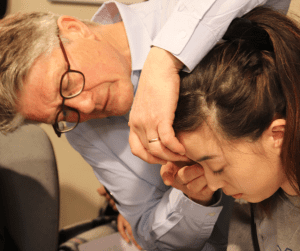
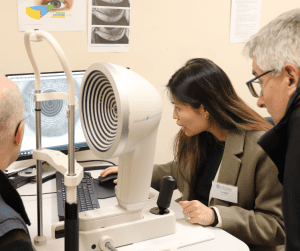
The ACO has always been, and continues to be, at the forefront of excellence in paediatric eyecare. Led by optometrists with expert training in their field, the Children’s Clinic employs state-of-the-art equipment and techniques to assess each case. Treatment plans are always tailored to individuals based on the best evidence practice to achieve the optimal health outcome.
This dedication to clinical excellence is matched only by its commitment to public health optometry. The not-for-profit organisation feels strongly that cost should not deter families accessing the eyecare a child requires, including access to advanced care such as axial measurement available through the ACO’s Myopia Clinic. Many of the ACO’s services are heavily subsidised and provided at a lower cost, including myopia control options.
Zeinab Fakih, ACO Manager of Paediatric and Rehabilitation Services, played a significant role in securing the extension of bulk billing for all children aged under eighteen years.
She commented, “We are thrilled to be extending bulk billing to include all paediatric examinations at the ACO. We are very aware that risks to children’s eye health are increasing, particularly with the rising prevalence of myopia. Early intervention is essential to offer the best outcome for a child’s long-term eye health. Cost simply should not be a factor in whether a child can access eye care.”
Kylie Harris, ACO Director of Operations, said, “The decision to take this next step in removing financial concerns reflects the ethos of the ACO. We are committed to ensuring high quality, equitable eye care for everyone who needs it and as an organisation, we’ll always explore how to improve accessibility to our services.”
In addition to removing financial barriers, the ACO’s Children’s Clinic welcomes children with complex needs who may otherwise struggle to access care in other optometry settings. Equipped with highly trained optometrists, the public health paediatric clinic supports children with developmental or health conditions and special needs to access the care that they need.
Eye care professionals are reminded that referrals are not required to attend the ACO but are always welcome.
*For Medicare eligible consultations only*.